Clinical
Case 1
70-year-old male refractory to current treatment for psoriasis
Treated for psoriasis for 5 years:
- Topical treatments, light therapy, and biologics
- Partial response to each treatment, but subsequent worsening of skin symptoms
- Most recently treated with anti–TNF-α inhibitor, but skin symptoms persisted
Complete blood count (CBC) showed mild lymphocytosis
- Skin biopsies of multiple lesions were collected
- Full workup showed mild lymphocytosis
- Normal LDH levels
- Lymph nodes normal on palpation
- Punch biopsy of the skin lesions were reviewed by a dermatopathologist with expertise in cutaneous lymphomas
- Skin biopsy results were suggestive of Mycosis Fungoides
- Flow cytometry was ordered
Clinical workup and skin biopsies from multiple sites raised suspicion of Mycosis Fungoides
- Refractory to current psoriasis treatment
- Worsening skin symptoms despite intense skin-directed and systemic therapy
- Abnormal lab results
- Mild lymphocytosis
- Abnormal findings in skin biopsies, suggestive of Mycosis Fungoides
- NCCN Guidelines recommend flow cytometry at diagnosis of Mycosis Fungoides or Sézary Syndrome, as well as for any T2-T4 skin stage or any extracutaneous disease1
- Flow cytometry can help determine accurate staging, inform prognosis, and guide treatment approach. It also helps to establish baseline blood involvement, which can be monitored for changes over time2
- When ordering flow cytometry, it is important to specify suspicion of Mycosis Fungoides or Sézary Syndrome in the request
- Up to 1 in 5 patients with early-stage (IA-IIA) Mycosis Fungoides may have B1 blood involvement3
- T-cell panel for Mycosis Fungoides and Sézary Syndrome should include CD3, CD4, CD7, CD8, CD26, and CD454
- Mycosis Fungoides can mimic psoriasis or other inflammatory skin conditions3
- NCCN Guidelines recommend consultation with a specialist who has expertise in CTCL whenever Mycosis Fungoides or Sézary Syndrome is suspected1

Clinical
Case 2
40-year-old female diagnosed 2 years ago with early-stage Mycosis Fungoides currently experiencing skin progression
Initially diagnosed with stage IB Mycosis Fungoides, skin-only involvement, relapsed after most current therapy
- Patient was initially diagnosed with stage IB Mycosis Fungoides (T2, N0, M0, B0) 2 years ago
- Initially presented with lesions over approximately 10% of skin surface
- Flow cytometry at diagnosis showed no blood (B0) involvement
- No evidence of extracutaneous involvement
- Patient was treated with phototherapy and bexarotene
- Skin symptoms were well controlled for ~1 year
Increasing extent of patches and plaques, and development of new tumors
Patient has not reported any constitutional symptoms
- Patient developed worsening skin symptoms
- Increasing extent of patches and plaques now covering >25% BSA
- Recently developed skin tumors indicating disease progression to stage IIB (T3)
Full workup showed enlarged lymph nodes
- CBC showed normal WBC
- Enlarged axillary lymph nodes on palpation
- Imaging and biopsy of lymph node showed enlarged lymph nodes (2-3 cm) with increased SUV uptake, and dermatopathic changes with small clusters of abnormal medium-sized lymphocytes—all suggestive of disease progression
- Skin biopsies were taken of the tumors and other lesions
- Blood sample was taken for flow cytometry
- Both the blood sample and the skin biopsies were sent together to the same lab to test for clonality and to evaluate whether there were matching T-cell clones in the blood and skin
- Flow cytometry showed progression to blood, with B1 classification bordering on B2 (950 cells/μL)
Clinical workup and lab results prompted concerns of disease progression to blood.
For consistency, the sample was sent to the same flow center that made the initial diagnosis for this patient in order to minimize variability due to differing methodologies across centers.
- Worsening skin symptoms
- Increase in extent of affected skin (>25% body surface area)
- Change in lesion type (patch/plaques → tumor)
- Lymphadenopathy, suggestive of extracutaneous disease
- Up to 1 in 3 patients with Mycosis Fungoides may progress to later-stage disease, which can affect skin, lymph nodes, blood, or other systemic compartments6
- Consensus guidelines from an international group of cytometry experts recommend flow cytometry for any patient that develops signs of disease progression2
- NCCN Guidelines recommend a multidisciplinary team approach with CTCL specialists for optimal management of patients with Mycosis Fungoides or Sézary Syndrome when possible1
- For consistency, send samples to the same flow cytometry lab

Clinical
Case 3
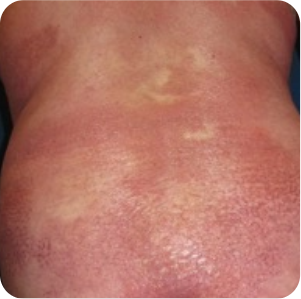
60-year-old male diagnosed 4 years ago with erythrodermic Mycosis Fungoides with low-level (B1) blood involvement whose treatment has stopped working
Initially diagnosed with stage IIIB Mycosis Fungoides with low-level blood involvement no longer responsive to photopheresis and pegylated interferon treatment
- Patient was initially diagnosed 4 years ago with stage IIIB erythrodermic Mycosis Fungoides with low-level blood involvement (T4, N0, M0, B1)
- Presented with diffuse erythroderma over 80% of body surface area
- Flow cytometry showed B1 blood involvement, with no evidence of nodal or metastatic disease
- Most recent treatment was extracorporeal photopheresis and pegylated interferon
- A skin PR was maintained for ~12 months, but efficacy is waning
Worsening skin symptoms with intractable pruritus and erythroderma, newly developed patches and acral fissuring and hyperkeratosis on his hands and feet
Flow cytometry showed rising blood involvement and a repeat flow test was scheduled
- Because of abnormal flow at baseline (B1 blood involvement), patient has been routinely monitored to assess for disease progression; until now, blood involvement had been stable since diagnosis
- For consistency, current blood sample was sent to the same lab that processed the previous samples
- Flow results showed increased blood involvement from baseline, with progression to B2 (3500 Sézary cells/µl)
- Patient started on a new systemic therapy, and a monthly blood analysis was initiated to monitor response to therapy
Blood involvement is routinely monitored in this patient because of abnormal flow results at diagnosis. At this visit, the clinical workup indicated signs of disease progression.
- Symptoms and/or signs of disease progression:
- Intractable pruritus
- Worsening erythroderma
- Mild lymphadenopathy
- Fatigue and malaise
- Refractory to current treatment
- Abnormal flow results at diagnosis
Blood involvement can develop at any stage and is associated with poor outcomes.5,6
Consensus guidelines recommend flow cytometry routinely (eg, every 3 months if feasible) for patients who have abnormal flow results at baseline. Flow can help monitor response to treatment and helps guide treatment approach.2

Clinical
Case 4
50-year-old female diagnosed 5 years ago with early-stage Mycosis Fungoides, recently developed serious skin infection
Initially diagnosed with stage IB Mycosis Fungoides with no blood involvement; currently treated with interferon-α
- Patient was initially diagnosed 5 years ago with stage IB to monitor response to therapy with patch lesions affecting 25% of body surface area (T2, N0, M0, B0)
- Flow cytometry showed no blood involvement; no other evidence of extracutaneous disease
- Treated with skin-directed therapies, then interferon; initial skin PR, but response subsequently waned
- Switched to an HDAC inhibitor and achieved PR
Worsening of patches, plaques, and itchiness, and enlarged lymph nodes
- Recently developed worsening pruritus and a severe skin infection that required hospitalization and IV antibiotics
- Worsening skin lesions affecting >30% of BSA, including thick plaques with yellow serous exudate
- Enlarged lymph nodes
Skin culture positive for S. aureus, and elevated WBCs with mild neutrophilia
- Skin and nasal swab cultures positive for Staphylococcus aureus (staph) infection
- Elevated WBCs with mild neutrophilia
Skin infection prompted concerns that the disease may be impacting immunity, and that, along with abnormal clinical findings, were suggestive of disease progression.
- Potential signs of disease progression and evidence of extracutaneous disease:
- Staph infection
- Worsening patches and plaques (T2)
- Enlarged lymph nodes
Patients with Mycosis Fungoides and Sézary Syndrome may have impaired immunity and increased risk of infection.7-9 NCCN Guidelines recommend flow cytometry for any patient with T2-T4 skin stage or evidence of extracutaneous disease.1 Additionally, recently published consensus website has guidance recommend flow cytometry when there are signs of disease progression or abnormal lab results. 2

Clinical
Case 5
50-year-old male, initially diagnosed with stage IA Mycosis Fungoides 5 years ago
Patch lesions affecting ~5% of BSA. Treated with phototherapy and topical steroids
- Patch lesions affecting ~5% of BSA at initial presentation
- Lymph nodes were normal on palpation
- CBC was normal with no signs of lymphocytosis
- Flow cytometry did not identify an abnormal T-cell population
- Treatment with phototherapy and topical steroids was effective
- Follow-up once a year, which included a full workup and flow cytometry
Flow cytometry showed an increase in blood involvement
- Flow cytometry was repeated
- Flow cytometry revealed an increase in blood involvement, correlating with B1 (low-level) classification
- Detection of an abnormal T-cell population in blood
Worsening skin symptoms, along with the increase in blood involvement and detection of an abnormal blood clone, may warrant closer follow-up.
- Worsening skin symptoms, suggestive of disease progression
- On diagnosis of Mycosis Fungoides, both a complete blood count and flow cytometry can provide a more complete diagnostic picture
- Mycosis Fungoides is often indolent, but up to a third of patients may experience progression within skin or to other disease compartments, including blood6
- Flow cytometry at diagnosis and throughout treatment is recommended to establish baseline, monitor disease progression, and help guide treatment approach1,10
- Upon signs of progression, flow should be performed and repeated routinely, every 3-6 months depending on the signs and symptoms and disease acceleration2

References: 1. Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Primary Cutaneous Lymphomas V2.2025. © National Comprehensive Cancer Network, Inc. 2023. All rights reserved. Accessed March 5, 2023. To view the most recent and complete version of the guideline, go online to NCCN.org. 2. Vermeer MH, Moins-Teisserenc H, Bagot M, et al. Flow cytometry for the assessment of blood tumour burden in cutaneous T-cell lymphoma: towards a standardized approach. Br J Dermatol. 2022;187(1):21-28. 3. Scarisbrick JJ, Quaglino P, Prince HM, et al. The PROCLIPI international registry of early-stage mycosis fungoides identifies substantial diagnostic delay in most patients. Br J Dermatol. 2019;181:231-232. 4. Horna P, Wang SA, Wolniak KL, et al. Flow cytometric evaluation of peripheral blood for suspected Sézary syndrome or mycosis fungoides: international guidelines for assay characteristics. Cytometry B Clin Cytom. 2021;100(2):142-155. 5. Olsen E, Vonderheid E, Pimpinelli N, et al. Revisions to the staging and classification of mycosis fungoides and Sézary syndrome: a proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC). Blood. 2007;110(6):1713-1722. 6. Agar NS, Wedgeworth E, Crichton S, et al. Survival outcomes and prognostic factors in mycosis fungoides/Sézary syndrome: validation of the revised International Society for Cutaneous Lymphomas/European Organisation for Research and Treatment of Cancer staging proposal. J Clin Oncol. 2010;28(31):4730-4739. 7. Hoppe RT, Kim YH. Clinical manifestations, pathologic features, and diagnosis of mycosis fungoides. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-pathologic-features-and-diagnosis-of-mycosis-fungoides. Updated September 23, 2022. Accessed October 24, 2022. 8. Krejsgaard T, Odum N, Geisler C, et al. Regulatory T cells and immunodeficiency in mycosis fungoides and Sézary syndrome. Leukemia. 2012;26:424-432. 9. Talpur R, Bassett R, Duvic M. Prevalence and treatment of Staphylococcus aureus colonization in patients with mycosis fungoides and Sézary syndrome. Br J Dermatol. 2008;159:105-112. 10. Olsen EA, Whittaker S, Willemeze R, et al. Primary cutaneous lymphoma: recommendations for clinical trial design and staging update from the ISCL, USCLC, and EORTC. Blood. 2022;140(5):419-437.